A research group led by Kobe University Graduate School of Medicine Project Professor MORIOKA Ichiro and Professor IIJIMA Kazumoto (Department of Pediatrics) has suggested a potential method of screening for jaundice (hyperbilirubinemia), a cause of cerebral palsy and loss of hearing in preterm infants, using painless dermal monitoring. The group also determined the correct area of skin to monitor for accurate results. This study has expanded the possibilities for accurate methods of monitoring jaundice, and it is hoped that this will lead to a decrease in cerebral palsy and hearing loss in preterm infants. The results of this research were published on 23rd September 2015 in the online version of The Journal of Pediatrics.
Japan has the world’s highest survival rate for preterm infants, thanks to advanced medical treatment and the availability of Neonatal Intensive Care Units (NICU). Despite this, cases of cerebral palsy and hearing loss caused by neonatal jaundice continue to occur, with cases reported for at least 2 in every 1000 infants born before the 30th week of gestation. It has also been established that cases of jaundice can worsen even two weeks after birth, meaning that there is a need for continuous long-term monitoring of infants in the NICU. However, jaundice in preterm infants is difficult to detect through physical observation, and monitoring through a daily blood test is not a realistic option.
Professor Morioka’s research group focused on transcutaneous jaundice monitoring used in daily health tests for full term infants. They monitored the bilirubin levels of 85 infants with a birth weight of under 1500 grams in NICUs at Kobe University, Kakogawa City Hospital, Hyogo Prefectural Kobe Children’s Hospital, Japanese Red Cross Society Himeji Hospital, and Takatsuki General Hospital. The research group took a total of 383 measurements. Through their results they were able to ascertain that the chest and back areas of preterm infants have the highest levels of sensitivity, and bilirubin levels in those areas were close to bilirubin levels in the blood.
In addition to expanding the possibilities for transcutaneous monitoring of jaundice in preterm infants, they discovered the optimum area of skin to monitor. This means that neonatal jaundice levels can now be monitored continuously using a painless method over a long period of time. It is hoped that this discovery will contribute to a decrease in cerebral palsy and hearing loss in preterm infants. Project Professor Morioka stated, “Even among paediatricians, many assume that neonatal jaundice is no longer an issue, but there are still many unknown factors regarding the effects of the illness on developing brain cells. I want to prevent after-effects such as cerebral palsy and hearing loss by providing effective jaundice monitoring for preterm infants.”
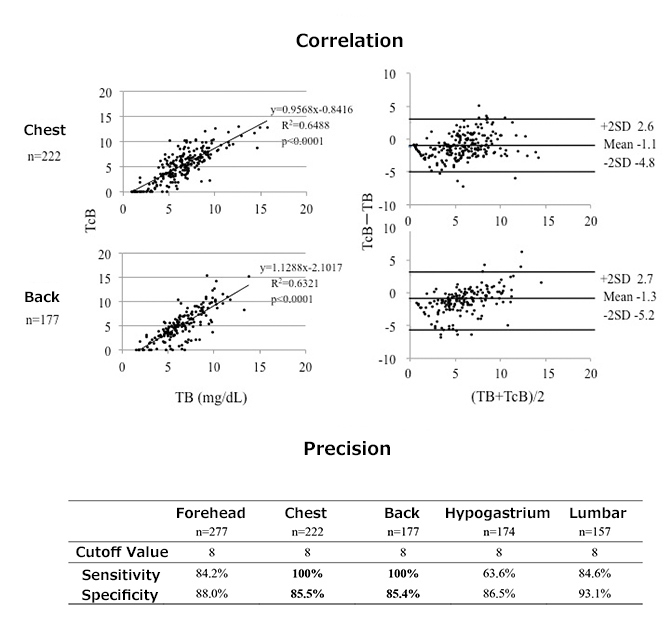
TB: Bilirubin in the blood, TcB: Transcutaneous bilirubin The levels of TcB in preterm infants differ depending on which part of the body is monitored. In order to detect the 10mg/dL level TB that indicates treatment for jaundice is necessary, the research group proposed that measuring the chest and back areas for levels of TcB of 8 or higher can be used as an accurate screening method for jaundice.
Journal information
- Title
- "Screening for hyperbilirubinemia in Japanese very low birthweight infants using transcutaneous bilirubinometry"
- DOI
- 10.1016/j.jpeds.2015.08.038
- Journal
- The Journal of Pediatrics