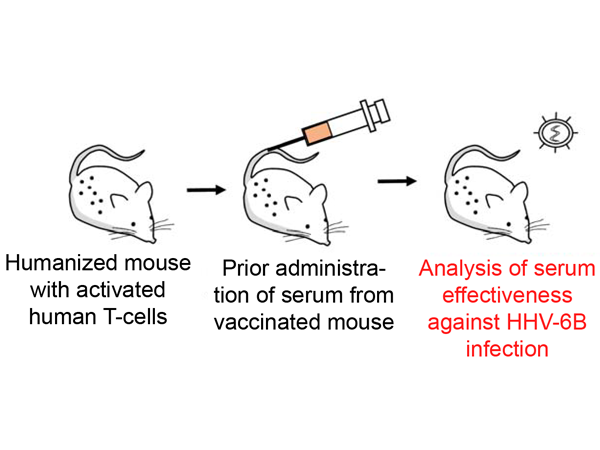
Mice with human immune cells are a new way of testing anti-cancer drugs targeting the immune system in pre-clinical studies. Using their new model, the Kobe University research team successfully tested a new therapeutic approach that blindfolds immune cells to the body’s self-recognition system and so makes them attack tumor cells.
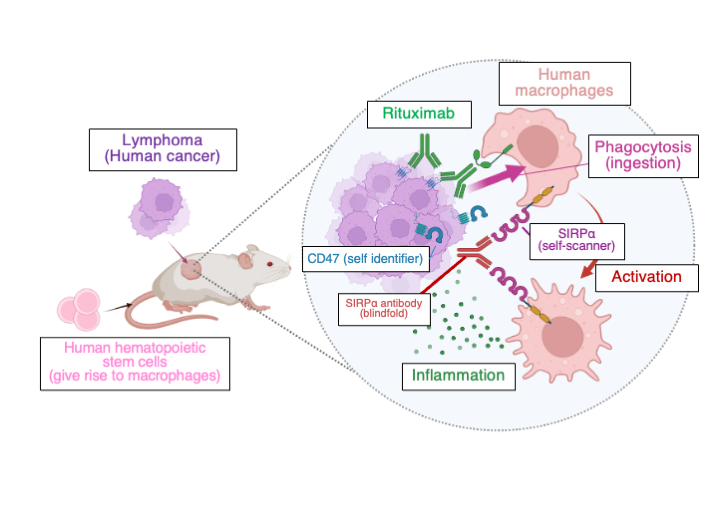
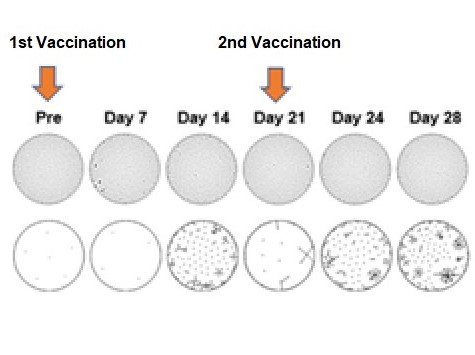
Cancer cells display structures on their surface that identify them as part of the self and thus prevent them from being ingested by macrophages, a type of immune cell. Cancer immunotherapy aims at disrupting these recognition systems. Previous studies showed that a substance that blinds macrophages to one of these identifiers, called “CD47,” by disabling their CD47-scanning structure, “SIRPα,” can activate the cells to fight the tumor when given in combination with therapeutic cancer-targeting antibodies such as Rituximab. However, because this approach is so specific to the self-identification of human cells, until now it could only be tested in humans or monkeys, making pre-clinical studies in mice impossible.
To overcome this, Kobe University immuno-oncologist SAITO Yasuyuki and his team built on their experience with creating mouse immunological models and transplanted parts of the human immune system into mice. Saito says, "Studies using mouse models with humanized immune systems have focused on lymphocytes, a type of immune cell relevant to infectious diseases. The special aspect of our approach is that our new mouse model focuses on macrophages because we want to target them for the development of new cancer immunotherapies." This enabled the researchers to both create a more fully functioning mouse model of human cancer and test the effectiveness of the blindfolding approach for the first time in this environment.
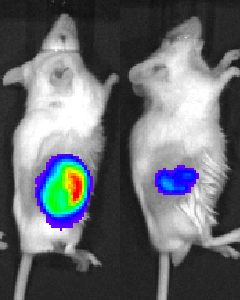
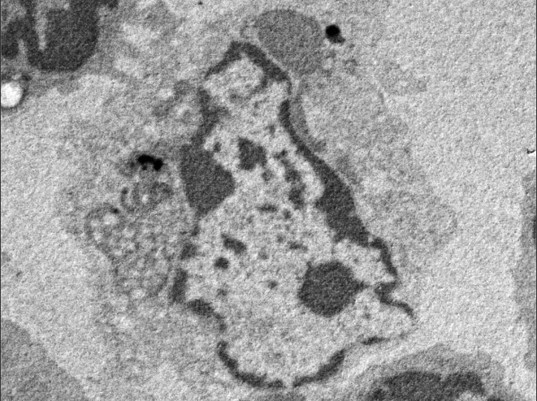
Their results, published in the journal Frontiers in Immunology, showed that the macrophage-targeted therapy indeed induced an effective cancer response. However, Saito explains, "The most exciting aspect of this result is that this approach not only promotes the engulfment (ingestion) of tumor cells by macrophages but also reprograms tumor-associated macrophages, one of the current topics of cancer immunotherapy."
The immune system has an ambiguous role in the development of and fight against cancer. On the one hand, it can recognize cancer cells and fight them. On the other hand, macrophages also associate with tumors, both supporting their growth and suppressing other anti-tumor immune responses. To turn these cells against cancer is the novel approach that the Kobe University researchers could now help propel forward with their new humanized mouse model.
But the result has a broader relevance, too. Saito says, "There were no suitable preclinical in vivo models to develop therapeutics targeting human macrophages surrounding tumors, so new approaches had to be tested directly on patients. I believe our model perfectly fills the gap and may help in the selection of the most effective treatment from several candidates for therapeutics targeting human immune cells. The long-term goal of my project is to develop a humanized immune system mouse model that faithfully represents the immune response against the tumor."
Acknowledgements
This study was supported by the Ministry of Education, Culture, Sports, Science, and Technology of Japan Grant-in-Aids 20K21547, 21H04807 and 20K16358; by Japan Agency for Medical Research and Development (AMED) grants 21cm0106308h0006 and 22674074; by Japan Science and Technology Agency (JST) grant JPMJPF2018; by the Bristol-Myers Squibb Foundation, the Takeda Science Foundation, and by the Japanese Society of Hematology. It was conducted in collaboration with researchers from the University and University Hospital Zurich and the Comprehensive Cancer Center Zurich.
Original publication
Y. Saito et al.: Preclinical evaluation of the efficacy of an antibody to human SIRPα for cancer immunotherapy in humanized mouse models. Frontiers in Immunology (2023). DOI: 10.3389/fimmu.2023.1294814
Release on EurekAlert!
Mice with humanized immune systems to test cancer immunotherapies