Clinical Fellow KONDO Atsushi and Professor NOZU Kandai et al. of Kobe University’s Graduate School of Medicine have estimated the prevalence of Gitelman syndrome across different ethnicities using a genome database. Their findings indicate that Gitelman syndrome is more common in the majority of ethnic groups than previously reported, with a prevalence ranging from 0.012 to 0.8 per 1,000 people. In particular, the prevalence was much higher in the Japanese population at approx. 1.7 per 1,000 people. This is far greater than the previously reported rate (approx. 1 in 40,000).
Although Gitelman syndrome is not generally recognized as a serious disorder that endangers the patient’s life, sufferers experience symptoms such as fatigue, which can hinder their daily activities and significantly reduce their quality of life. In rare cases, it can be accompanied by extrarenal complications including arrhythmia.
As a blood test is necessary to diagnose Gitelman syndrome, it is likely that many patients with this syndrome do not receive the correct diagnosis even if they display symptoms.
These research results were published in Scientific Reports on August 9, 2021.
Main points
- Gitelman syndrome is an inherited tubulopathy (*1). Manifestations include fatigue, muscle weakness, nocturia and cravings for salt. Symptoms are non-specific and can reduce sufferers’ QOL (*2). Gitelman syndrome is sometimes accompanied by extrarenal complications, such as arrhythmia, that can be fatal.
- Gitelman syndrome is said to have a prevalence rate (*3) of 1 in 40,000 people and at least 1% are carriers (*5). However, a complete picture of the epidemiology of this syndrome has yet to be illuminated.
- In this study, the researchers estimated the prevalence of Gitelman syndrome using multiple genome databases and found that the prevalence rate for many ethnicities was higher than previously reported. In particular, they showed that for those of Japanese ethnicity, it was far higher than other ethnicities at a rate of approximately 1.7 per 1,000 people.
- These results indicate that there are probably many people with Gitelman syndrome who have not been diagnosed correctly and therefore cannot receive appropriate treatment, even though they have symptoms which impact their daily lives.
Research Background
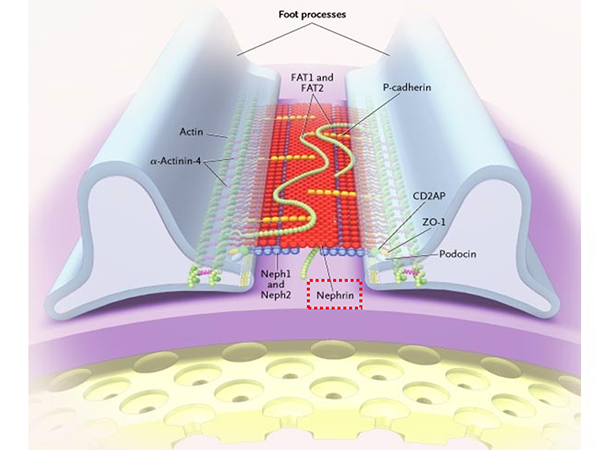
Gitelman syndrome is a salt-wasting tubulopathy and an autosomal recessive inherited disorder (*4) caused by mutations in the gene SLC12A3. It has been said that 1% carry pathogenic variants of this gene and that 1 in 40,000 people have Gitelman syndrome, however an accurate prevalence rate has yet to be determined.
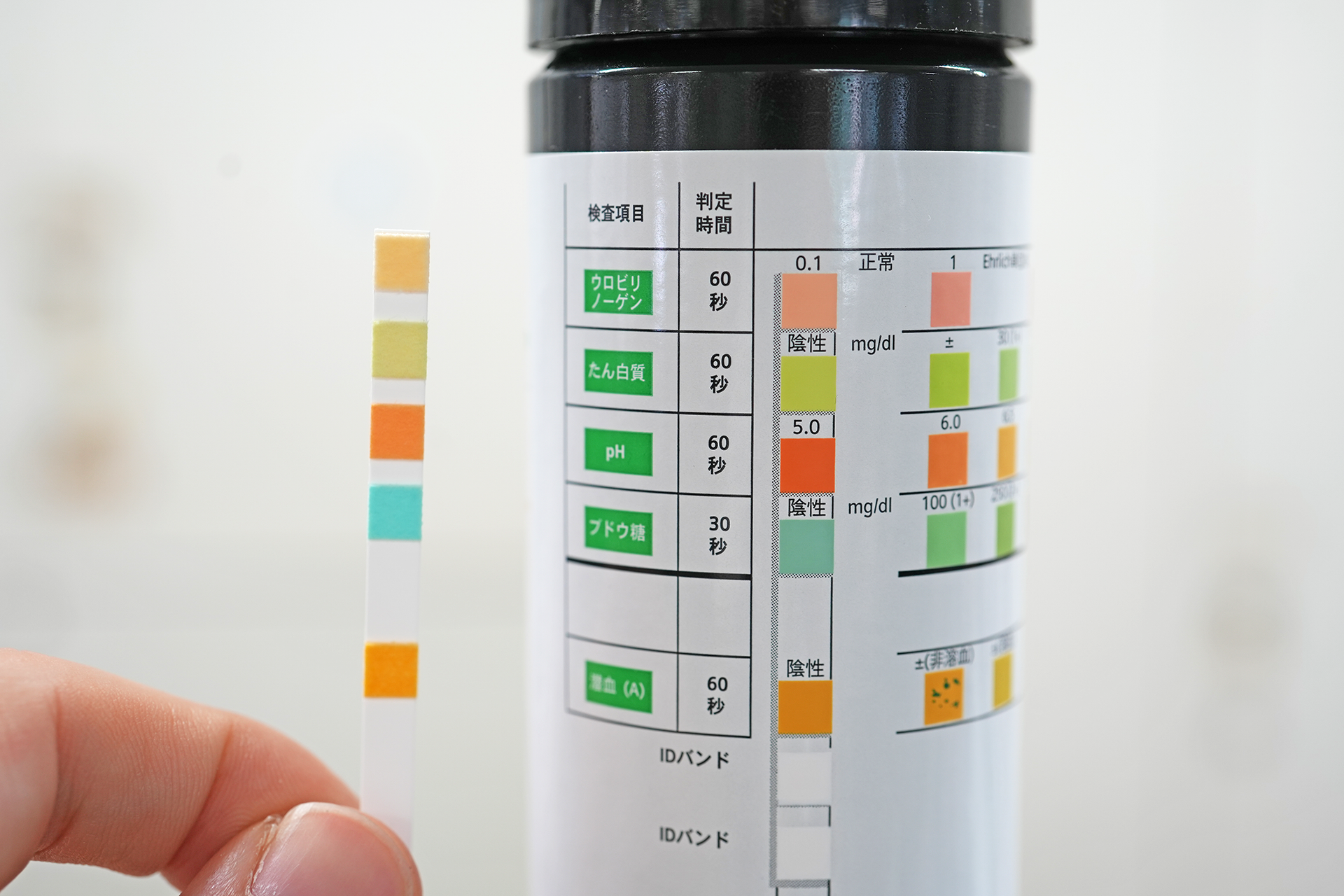
Even though those with Gitelman syndrome have a good life expectancy, they experience symptoms that decrease their QOL, such as fatigue, muscle weakness, nocturia and salt cravings because their kidneys are unable to regulate the electrolyte balance for mineral ions in the blood, such as potassium. In some cases, sufferers exhibit fatal arrhythmia. However, Gitelman syndrome does not have any specific symptoms and requires a blood test to be correctly diagnosed. Therefore, it has been predicted that there are many patients who do not receive appropriate treatment.
The members of this research team have seen many cases where Gitelman syndrome was undiagnosed. This includes cases where the patient was misdiagnosed with a psychological disorder, and where the patient was not aware that they were ill despite experiencing significant fatigue. This indicates that there are numerous cases where the patient suffers for many years but is unable to obtain the correct diagnosis and treatment. The team conducted this research in the hope that if they could ascertain that the true prevalence of Gitelman syndrome is higher and thus more common than previously reported, then this greater understanding could contribute towards its early diagnosis and treatment.
Research Methodology and Findings
Method
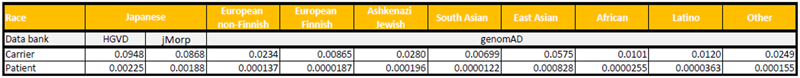
The researchers selected all of the missense (*6) and nonsense mutations (*7) of the SLC12A3 gene registered as pathogenic genetic variants in HGMD® Professional (The Human Gene Mutation Database); for a total of 247 variants. Among this number they looked at the 140 variants for which the allele frequency (*8) across different ethnicities had been publicized in multiple online genome databases (HGVD, jMrop, gnomAD), and calculated the total allele frequency for these variants. Assuming that the Hardy-Weinberg Principle (*9) applies, if the aforementioned total allele frequency is represented by q, then the carrier frequency was estimated to be 2q and the prevalence rate q2 under autosomal recessive inheritance. Based on this theory, the researchers calculated the percentages for each ethnicity.
Results
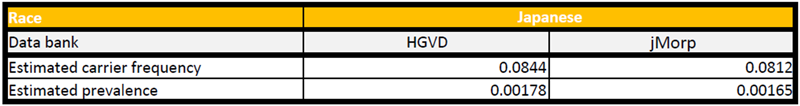
1. The estimated carrier frequencies for these variants was around 9% in Japanese people, and ranged from 0.7% to 5.8% in other ethnicities. In addition, the estimated prevalence per 1,000 people was found to be around 2 for Japanese ethnicity and between 0.012 and 0.8 for all others (Table 1).
2. The reason that the estimated prevalence in Japanese people is higher than in other ethnicities is believed to be due nine variants that have particularly high allele frequency in Japanese people (allele frequency ≧0.001). It has yet to be confirmed whether or not three of these nine variants cause Gitelman syndrome. If these three unconfirmed variants are excluded, then the estimated carrier frequency in Japanese people is around 8% and the prevalence rate is approx. 1.7 per 1,000 people.
3. The research group conducted a retrospective data analysis study using patients’ electronic records to assess the validity of the above research results. They selected Kobe University Hospital outpatients aged 16 to 30 who had undergone blood tests including the serum potassium level between January 1, 2010 and December 31, 2020 (a total of 14,335 patients). Of this number, 143 people had low serum potassium levels (below 3.1mEq/L) and clear causes other than Gitelman syndrome could not be determined in 13 cases.
These results show that 0.9 in 1,000 outpatients at the hospital have possible Gitelman syndrome. This is lower than the above estimated prevalence rate, however it is predicted that even more patients with this syndrome would be identified if the criteria for the study (target age range and serum potassium levels) were widened. Therefore it was concluded that the results do not significantly contradict each other.
Further Research
Database accuracy is important for this research, so it is hoped that more genetic information can be collated. Gitelman syndrome cannot be diagnosed if it is not tested for, leading to cases where it is overlooked even if the patient is experiencing symptoms such as fatigue that impact their daily life, as well as cases where the patient is unaware that their symptoms are the result of an illness. These research results have indicated that there are many people with potential Gitelman syndrome. This will hopefully contribute towards enabling these people to receive the correct diagnosis and treatment, improving their QOL.
Glossary
- *1 Tubulopathy
- Renal tubules are minute tubes in the kidneys that reabsorb necessary substances such as water, minerals and sugar from the glomerular filtrate (substances filtered from the blood as the first step in urine formation), thus regulating the balance of minerals and keeping the amount of water in the body constant. A tubulopathy is a disease that affects these tubules.
- *2 QOL
- This stands for ‘Quality of Life’ and indicates a patient’s overall satisfaction with their life, including physical and mental aspects, and social activities.
- *3 Prevalence rate
- The percentage of people with a certain disease at a certain point in time.
- *4 Autosomal recessive inherited disorder
- The gene that causes a particular disorder is located on an autosome (numbered chromosome). The disorder develops if both genes in the pair have a mutation.
- *5 Carrier
- Someone who carries the genetic mutation that causes a disorder but doesn’t have the disorder itself. In the case of Gitelman syndrome, the carrier has a mutation in just one of the pair of causal genes.
- *6 Missense mutation
- The substitution of a single base pair for a gene which results in a different amino acid being translated at that position.
- *7 Nonsense mutation
- A genetic mutation that prematurely stops protein synthesis.
- *8 Allele
- An allele refers to a version of an individual gene which has two or more variants that can occur at the same location on the chromosome. Humans inherit two alleles for each gene, one from each parent.
- *9 Hardy-Weinberg Principle
- The principle that allele frequency (genetic variation) will remain constant from generation to generation if mating is random in a significantly large population.
Acknowledgements
This research received funding from: a Health and Labor Sciences research grant for ‘Research, diagnosis and treatment of childhood-onset, rare, and intractable kidney diseases’ from the Ministry of Health, Labour and Welfare of Japan (grant no. 20FC1028), and a KAKENHI grant from the Japan Society for the Promotion of Science (JSPS) (grant no. JP19K08726).
Journal Information
- Title
- “Examination of the Predicted Prevalence of Gitelman Syndrome by Ethnicity Based on Genome Databases”
- DOI
- 10.1038/s41598-021-95521-6
- Authors
- Atsushi Kondo1*, China Nagano1, Shinya Ishiko1, Takashi Omori2, Yuya Aoto1, Rini Rossanti1, Nana Sakakibara1, Tomoko Horinouchi1, Tomohiko Yamamura1, Sadayuki Nagai1, Eri Okada1, Yuko Shima3, Koichi Nakanishi4, Takeshi Ninchoji1, Hiroshi Kaito1, Hiroki Takeda1, Hiroaki Nagase1, Naoya Morisada1, Kazumoto Iijima1, Kandai Nozu1
1) Department of Pediatrics, Kobe University Graduate School of Medicine.
2) Clinical and Translational Research Center, Kobe University Hospital.
3) Department of Pediatrics, Wakayama Medical University.
4) Department of Child Health and Welfare (Pediatrics), Graduate School of Medicine, University of the Ryukyus
*Corresponding author - Journal
- Scientific Reports