On May 8, Japan’s government reclassified Covid-19 as a “Class 5” disease according to the Infectious Diseases Control Law, putting it on the same level as the seasonal flu. This comes three years and four months after the first infections were confirmed in Japan, signaling a transition from a state of emergency to a non-emergency in terms of the response to Covid-19. What have we learned from this pandemic that has lasted over three years? What kinds of changes will this transition bring, and what issues will we continue to face? We asked Professor MORI Yasuko of the Division of Clinical Virology at Kobe University Graduate School of Medicine’s Center for Infectious Diseases.

With the World Health Organization (WHO) ending its declaration of a state of emergency on May 5, it would appear that we have turned a corner in this pandemic. As an expert in the field of infectious diseases, what do you feel we have learned from these three years of Covid-19 pandemic response?
Professor Mori:
We were forced to face the fact that being caught off guard by an infectious disease capable of causing a global pandemic, especially a virus capable of airborne infection, could lead to a global pandemic on a scale that humanity has never seen before. As a specialist on infectious diseases, I thought I knew this on some level, but this pandemic has raised my awareness to new heights. Most researchers were not able to predict the degree to which this virus would spread across the globe, causing high numbers of deaths and serious illness when the first cases were reported in China in December of 2019.
At the same time, it’s also amazing that a viable vaccine was produced in such a relatively short time. Typically, the safety of vaccines is paramount, and the approval process takes years. In contrast, the Covid-19 vaccines were developed quickly while people’s lives were hanging in the balance, making them something of a “field vaccine.” The vaccines were able to be developed so quickly in the U.S. thanks to the messenger RNA research that had already been done by the time vaccine development began, and the fact that researchers there got to work early using that research. These are some of the lessons that we saw other countries doing and that Japan would do well to incorporate into our preparedness for the next potential pandemic.
Carry forward what we’re learned—it’s not over yet
How would you assess Japan’s response to the Covid-19 pandemic?
Professor Mori:
On this reclassification as Class 5 specifically, I think the government could actually have made that decision even earlier. Looking at other examples outside Japan makes me think that perhaps we should have considered getting society and the economy running again sooner. But this was all the first time we’ve had to deal with Covid-19, so all we could do was try things out and see. The important thing to remember, however, is that this doesn’t mean that it’s over, but we already have a lot of things we’ve learned for next time.
One example of a lesson we’ve learned is that we need to continue to push toward digitalization in areas like understanding data on infectious diseases, getting information out, and collaboration between medical facilities to facilitate a smoother response.
What major changes will we see with the change to Class 5?
Professor Mori:
One big difference is that people will be able to be seen at more different medical facilities than before. Things may not change overnight, but we’re also going to see restaurants and bars return to their normal operating hours and people’s lives will be freer in general.
At the same time, it’s essential that we continue to protect the elderly and other people who are at higher risk. Being changed to Class 5 doesn’t mean that the virus is going away. In fact, it will be even more important for people as individuals to keep it in mind. In spite of the costs, people need to have testing kits, pulse oximeters, and other tools ready. If you have symptoms, stay home as much as you can, and wear a mask, and if you are at higher risk should see a doctor right away. These are the things we need to keep in mind going forward.
Transition away from emergency handling of vaccines
The reclassification of Covid-19 as Class 5 brought with it the end of notifiable disease surveillance, and infections will be monitored based on sentinel surveillance, which will be reported based on figures from designated medical facilities. Will this make it more difficult to understand trends in infection in a timely manner?
Professor Mori:
Our understanding of conditions maybe be somewhat slower than before, but we also track infections of seasonal influenza using this same sentinel surveillance. What’s crucial is that both the national and local governments continue to conduct surveys of Covid-19 infections so that we can respond rapidly if there is an increase in infection numbers. This also allows us to discover new variants of the virus earlier. As researchers, we will continue to conduct surveys as well.
| Infectious diseases | |
|---|---|
| Class 1 | Ebola, bubonic plague |
| Class 2 | Tuberculosis, SARS |
| Class 3 | Cholera, shigellosis, typhoid fever |
| Class 4 | Rabies, malaria |
| Class 5 | Seasonal flu, syphilis |
The national government plans to consider incorporating the vaccine into immunization schedules. What are your thoughts on this?
Professor Mori:
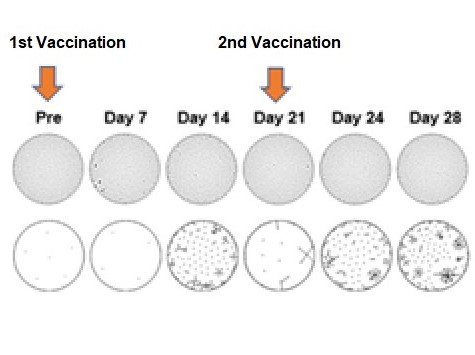
Last year we worked with Hyogo Prefecture announce the results of research indicating that a third round of vaccination was effective against the omicron variant, and have been recommending that people get vaccinated three or four times. With progress in vaccinations, many more people now have greater immunity, leading to the suppression of the spread of the virus that we see now.
Now that we are no longer under a state of emergency, however, there are doubts as to whether vaccinations should continue with the same vaccines that have been used so far. When the virus was continuing to spread, the top priority was to treat the virus, even if there were side effects such as fever. Nevertheless, vaccines should need to have basically no side effects, so we need to continue to develop vaccines that have none. This is something that we are able to work on now that the situation has calmed down.
Whether vaccinations should be continued with the current vaccines is a point that should continue to be discussed, which is another reason that continued monitoring of Covid-19 is still necessary.
Advanced research is key
Should we just expect that another pandemic could be caused by a different virus in the near future?

Professor Mori:
The current Covid-19 pandemic has reminded us that there are numerous viruses in the world that have never infected humanity to before. It may be a few years or a hundred years from now, we don’t know when, but another pandemic will happen.
“Advanced research” to discover new animal viruses before they make the jump to humans has become more prevalent recently. Some have said that the Covid-19 virus has its origins in bats, but we need to be able to discover these pathogens that may lead to the next pandemic and think about how to prevent infection by those pathogens in advance. This type of research is a crucial tool in preparing for new pandemics. Centers for infectious disease research have been established across Asia and Africa by the Japan Agency for Medical Research and Development (AMED) and are currently surveying infections. Kobe University also has set up a research center for infectious diseases and will continue to survey infections there.
This fall, Japan will establish a new cabinet agency to manage pandemic response, and will also set up a Japanese version of the U.S. Centers for Disease Control (CDC) starting in 2025. Will these organizations function effectively?
Professor Mori:
Bringing together information on infections around the world and strengthening our systems for disseminating that information will be essential. We need to create a system that enables local governments to access that information and also report back to the national government on local trends quickly. Understanding these conditions earlier makes it possible to contain infections before they spread. Of course, such a system will also require cooperation between research, medical, and other institutions.
In order to disseminate information about Covid-19 infections, we worked with Hyogo Prefecture to provide information through a press conference with the governor, as well as using YouTube. We also received research funding from the prefecture. We hope to be able to use this experience to inform people about the results of our research with an emphasis on cooperating with local governments in the future as well.
Resume
| March 1998 | Completed PhD at Graduate School of Medicine, Osaka University |
| October 2001 | Assistant, Graduate School of Medicine, Osaka University |
| June 2003 | Assistant Professor, Graduate School of Medicine, Osaka University |
| April 2005 | Chief Project Lead, National Institute of Biomedical Innovation |
| April 2008 | Professor, Graduate School of Medicine, Kobe University |